Patella Conditions
What are patella conditions?
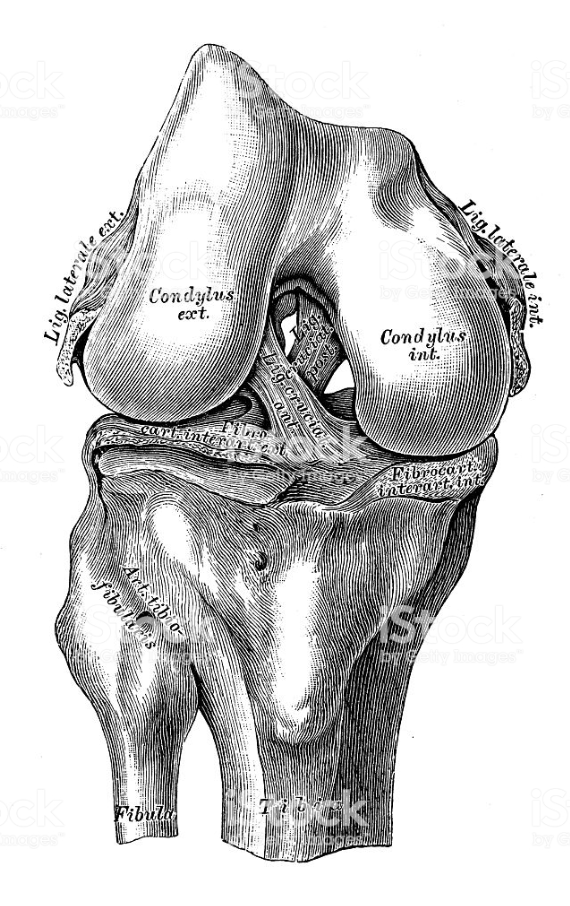
This is a very complicated area, as there are so many conditions that can affect the structure and functioning of the kneecap. The patella is wrapped inside a tendon that connects the strong muscles of the thigh (quadriceps) to the shin, and so the patella plays an important part in bending and straightening the leg. The part of the tendon above and around the kneecap is called the quadriceps tendon, and the part below the kneecap is called the patellar tendon.
The following are some of the more common patella conditions:
- Trauma – acute or repetitive traumas e.g. runner’s/ jumper’s knees, or Osgood-Schlatter Disease in adolescents
- Abnormalities in the structure and position of the kneecap, with lateral compression syndrome
- Instability of the patella, when the kneecap dislocates or slides
- Patella osteoarthritis
- Patella syndrome (often found in young female patients)
What causes them?
Trauma – a blow or injury to the knee (so-called acute trauma), or overuse syndromes (so-called repetitive trauma)
Structural abnormalities – usually congenital although they may be the result of arthritic changes
Instability of the patella – can be caused by a blow or it can be congenital or acquired.
Patella osteoarthritis – damage to the cartilage which causes changes in the underlying bone. This can develop as a result of abnormal contact between the patella and the femur, or with repeated dislocation or sliding (subluxation)
Patella syndrome – in younger patients it is often impossible to attribute a cause, but in older patients it can be a result of any of the above causes.
How does it feel?
In all these conditions you will feel pain on the front of the knee, and in some cases you may also feel pain at the back of the knee. Pain is typically increased by bending the knee (descending stairs), during sport, or after sitting down for a long time with a bent knee (watching a film, driving). There is sometimes swelling, although this is not indicative of a patella condition. You may often hear a clicking or creaking noise, and with patella instability, you may feel that the knee is giving way.
Diagnosis
Your doctor will make a physical examination of your knee, and he will ask for X-rays to exclude or confirm abnormalities of the shape or alignment of your kneecap. In the case of conditions that relate to the soft tissues of the knee, you will be asked to undergo an MRI (magnetic resonance imaging) scan. In some cases, your doctor may ask for a CT (computer tomography) scan of the whole limb to see if there are any abnormalities in the alignment of your hip and knee.
Treatment – conservative
There are various conservative treatments that can relieve patella conditions. Physiotherapy exercises can help to recondition your thigh muscles, and to stretch contracted tendons. Your doctor may prescribe pain killers, ice packs or anti-inflammatory medication. He may also prescribe hyaluronic acid injections, shock wave treatment, or a knee brace. Changes in lifestyle – such as losing weight, or regulating your sporting activity – can also help alleviate the symptoms.
Treatment – surgical
1. Arthroscopic Patella Realignment: In the cases of patella abnormalities and instability your surgeon can re-position the patella arthroscopically, or in more severe cases the surgeon may need to perform this procedure in open surgery.
2. Patella osteoarthritis normally occurs with arthritis of the whole knee (see the section on Knee osteoarthritis for details of the treatment). If the arthritis is limited to the patella femoral cartilage, the following treatments can be preformed:
Abrasion Arthroplasty: when the cartilage has worn away and bone rubs on bone, the bone-surface becomes hard and shiny. During arthroscopy, the surgeon can use a special instrument known as a burr to scrape off the hard, polished bone tissue from the surface of the joint. The scraping action causes a healing response in the bone, with new blood vessels entering the area, bringing stem cells, and causing the formation of scar tissue (fibrocartilage).
Arthroscopic Microfracture: the surgeon will clear away the damaged cartilage, and then use a blunt tool to poke a few tiny holes in the bone under the cartilage. Like abrasion arthroplasty this procedure is used to get the layer of bone under the cartilage to produce a healing response, triggering the formation of new cartilage (mainly fibrocartilage) inside the lesion.
Chondrocyte Transplant (cartilage graft): During arthroscopy the surgeon will remove a piece of healthy cartilage, which will then be put in culture. Over the next 4-6 weeks more cartilage cells will grow. These cells will then be re-injected into the lesion where they should adhere and replicate, creating new articular (not fibro) cartilage.
Partial Knee Replacement: In severe cases of arthritis, your surgeon will perform a partial knee arthroplasty in open surgery. He will remove the damaged bone from the patella and femoral surfaces, and replace this with a synthetic cap on the femur, and a button component on the patella surface. He will then align the joint and ensure that the knee bends and straightens correctly. After surgery, you should have a correctly aligned leg and a full range of motion. You will normally have to stay in hospital between 3 to 10 days, depending on your personal rate of recovery, and also on how difficult it will be to manage at home (stairs, assistance at home etc.).
Rehabilitation after surgery
Abrasion/Microfracture/Chondrocyte transplant: You should be able to walk reasonably normally, dosing your weight with the aid of crutches, but will have to avoid putting any pressure through a bent knee (i.e. going up and down stairs, walking on steep slopes, squatting etc) for 6-8 weeks. You will start physiotherapy immediately after the operation, with the first treatments designed to help control the pain and swelling from the surgery, and to make sure you are only putting a safe amount of weight on the affected leg. Then exercises will be introduced to help improve knee motion and to get the muscles toned and active again. At first, emphasis is placed on exercising the knee in movements that don’t strain the healing part of the cartilage. But as the program evolves, more strenuous exercises will be introduced.
Partial Knee Replacement: You will be able to walk almost immediately after the operation, although your doctor will prescribe crutches to help with balance and to make walking more comfortable, and he will give you light exercises to start rebuilding your quadriceps muscles. A physiotherapist will teach you how to get out of bed correctly, how to walk with crutches, and how to dose your weight according to the level of discomfort you feel. Most patients keep their crutches for about a month. The physiotherapy will become more strenuous as time passes in order to rebuild your muscles, and particular attention will be given to straightening the leg fully.
When will I be back to normal?
Ideally, patients will be able to resume their previous lifestyle activities. Some patients may be encouraged to modify their choice of activity.
Arthroscopic Microfracture/Abrasion Arthroplasty /Chondrocyte transplant: It could be 9-12 weeks before everyday activities become completely comfortable, although you can start driving after 15 days. The damaged area goes on developing for months after surgery, so certain sports may not be advisable during that period.
Partial Knee Replacement: Most patients return to work after about 2 months, although those who have a sedentary job may be abler to return quicker than this. Everyone is different and your doctor will be able to advise when your muscles are strong enough for you to return to work. You can start driving when the wound is healed (after about 2 weeks).