Ankle instability
What is ankle instability?
This condition refers to when the outside of your ankle continually gives way, particularly when you are walking on an uneven surface, or sometimes even if you are just standing.
When you sprain your ankle, the lateral (outer side) ligaments which hold the bones of the joint in place are stretched, or with a serious sprain are torn. Until they heal fully you will be unable to control the movement of your ankle joint, and regulate your balance. Therefore, if they do not heal correctly, the ankle is unstable and prone to giving way. Ankle instability is a vicious circle: when the ankle gives way, you will damage the ligaments, which will become weaker and more likely to give away again, causing more damage and further weakness… and so on. Additionally, patients with unstable ankles are more likely to suffer from other ankle conditions such as osteoarthritis, or impingement.
What causes it?
Ankle instability usually develops after an ankle sprain that has not healed properly, or if you have not rebuilt the muscles and got back your balance adequately after a sprain. Repeated ankle sprains can weaken and stretch the ligaments so that they are no longer able to hold the ankle joint in alignment.
How does it feel?
You will have persistent pain and swelling around the ankle – particularly on the outside – and it will be tender to the touch. Your ankle will give way, particularly when walking on uneven surfaces.
Diagnosis
Your doctor will ask you about your medical history and will make a physical examination of your ankle. He may ask for X-rays to rule out a fracture, and an MRI (magnetic resonance imaging) scan to evaluate the scale of the damage to the soft tissues.
Treatment – conservative
To reduce the pain and inflammation your doctor will prescribe anti-inflammatories. To prevent the ankle from giving way and causing further sprains he may advise wearing a plastic ankle brace, or special insoles in your shoes to stop the ankle rolling out wards. He will also ensure that you are wearing the correct type of shoes that support the ankle, and no high heels. He will also prescribe a course of physiotherapy to restore your muscle strength and co-ordination, and improve your range of motion.
However, if the instability persists, or where the ligaments have been completely torn, your surgeon may recommend surgery.
Treatment – surgical
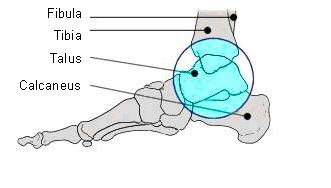
Tendon graft: if your ligaments are too damaged to be able to support your ankle, even if they are tightened and reinforced, your surgeon may take a section of one of the tendons that run around the ankle. Your surgeon will make a 4-5cm incision on the outside of your ankle, and make a hole in the fibula and the talus where the ligament attaches to the bone. He will then a remove a section of the tendon and thread it through the holes, attaching it with suture anchors or staples. Finally, he will close the incision with stitches.
Rehabilitation after surgery
You will be in a cast for about 3-4 weeks after the operation, and you may find crutches useful for the first few days whilst you get used to walking with the cast. Once the cast is removed you will start physiotherapy to regain your range of movement, to rebuild the shin and ankle muscles, and most importantly, to develop your balance and co-ordination to ensure that the ankle does not become unstable again. In the first few weeks after the cast is removed, you may find it more comfortable to wear an ankle brace for if you are doing strenuous weight bearing activity (e.g. walking long distances).
When will I be back to normal?
You will be able to drive after about a month. Office workers can return to work almost immediately, although manual workers will need to wait 45 days.
You can start light sports (cycling, swimming etc.) after about a month, and contact sports after 3 months, although you should wear an ankle brace initially.