Ankle arthritis
What is osteoarthritis?
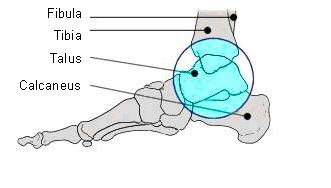
Osteoarthritis is the progressive degeneration of the articular cartilage that coats the end of the tibia and the surface of the talus. It is due to the cartilage that the bones can move smoothly against each other without causing friction, and thus damage to the bone surfaces. In the early stages of arthritis the cartilage layer becomes damaged and loses it’s elasticity and smoothness. In the later stages, holes appear in the cartilage, exposing the underlying bone. Without the protective layer of cartilage the bone hardens and produces bony protrusions, or spurs (called osteophytes) that deform the shape of the bones. The synovial membrane becomes chronically inflamed and produces excess synovial fluid which causes the ankle to swell. The joint capsule stiffens and limits the movement of the joint. Osteoarthritis is a disease that normally occurs in older patients, however ankle arthritis is often the result of a trauma and thus can affect younger patients.
What causes it?
There are various causes of osteoarthritis, but in the ankle it is most frequently caused by serious injuries or rheumatic diseases.
How does it feel?
The main symptom of osteoarthritis is pain. You will have pain in your ankle only after activity in the initial stages, and then more constantly as the condition develops – significantly limiting movement. Your ankle may swell and feel tight. Your ankle may make a squeaking or creaking noise when you move.
Diagnosis
Your doctor will ask you about your medical history and make a physical examination of your ankle, and other joints. He will ask for X-rays to see the state of the bones and to judge the degree of arthritic damage (as the cartilage wears away, the space between the bones in the joint becomes narrowed). In order to complete the diagnosis, your doctor may ask for an MRI scan or a CT scan.
Treatment – conservative
Your doctor may prescribe any, or all, of the following treatments:
- Change of lifestyle – for example losing weight, and regulating your level of activity
- Medication – chondro-protective (e.g. glucosamine, chondratin sulphate, or methyl methanesulfurnate), or anti-inflammatory medication
- Injection therapies such as hyaluronic acid or cortisone injections
- Shock wave or magneto therapy
- Physiotherapy – exercises to regain the range of movement of your ankle, to rebuild muscular strength, and to improve your balance.
- Change of footwear – using a shoe with a rounded ‘rocker’ sole may relieve the pain
Treatment – surgical
Arthroscopic Debridement: this is carried out on more minor damaged areas and is aimed at preventing or delaying further progression of the problem. The surgeon cleans up the joint, trimming any rough edges of cartilage or bone spurs, and removing loose particles of cartilage and bone. This procedure is sometimes referred to as chondroplasty.
Ankle Replacement: recent developments in prosthetic ankles have meant that this can be a highly successful solution to osteoarthritis. An ankle prosthesis is made up of 2 pieces; a tibial component which is a metal tray lined with a plastic cup or socket, and a talus component that fixes into the talus bone and hinges in the plastic socket. Your surgeon will make a 10cm incision on the front of your ankle exposing the soft tissues, which he will move aside and then open the joint capsule. Next he will shape the ends of the bone (at the same time removing the arthritic damage) to fit the new ankle components. Then the prosthesis will be fixed into place and tested to check that it works properly. Then the surgeon will fix the tibia and the fibula together so that they cannot move and dislodge the tibial component, and insert a bone graft between the 2 bones (using the bone removed when fitting the prosthesis) so that they fuse together. Finally your surgeon will sew up the joint capsule, and then the incision in the skin.
Arthrodesis or Fusion: in rare cases, the 2 bones may be fused together i.e. allowed to grow together to form one bone. Although the ankle will no longer move, you should still be able to move normally (with some limitations) and most importantly, without pain. The operation is similar to that described above for a prosthesis, apart from the fact that the space between the 2 bones is filled with pieces of bone (either your own, or from a donor) rather than the prosthetic components. The bones are held in place with 2 or 3 screws fixed internally, or by using an external metal frame which will be attached to the bones.
Rehabilitation after surgery
Debridement: you should be able to walk immediately after the operation, although you may find crutches helpful for the first few days.
Ankle replacement: you will need to wear a resin boot or rigid brace for 4 weeks, which should enable you to walk. You will need to go back to your doctor regularly with X-rays so that he can follow the healing process of your bones. During this time, you will do physiotherapy exercises to maintain the muscle tone in your leg, and then once the brace has been removed, you will need to do another 2-3 months of physiotherapy to regain the range of movement in your ankle, build up the muscles and ensure your ankle is stable.
Fusion: rehabilitation will depend on the type of fixation your surgeon has used. With an external frame, you will be encouraged to put weight on your foot immediately, and the frame will be removed (during a very short operation) after 8-12 weeks. If the surgeon has used internal screws, you will need to wear a resin boot or rigid brace for 45 days after surgery. Once the brace is removed you will begin physiotherapy to strengthen your muscles, using an ankle-brace for a further 3-4 weeks. You doctor will ask you to undergo an X-ray ever 30-45 days until the bones have completely fused together. Once you are fully weight-bearing, your physiotherapist will teach you to walk correctly and will give you exercises to strengthen your leg muscles, and improve your co-ordination and balance. A shoe with a ‘rocker’ curved sole, and insoles will help you walk normally.
When will I be back to normal?
Debridement: you can return to office work and after 2-3 days, to driving after a week, and to manual work after 2 weeks. You can start light sporting activity after 2 weeks, and weight-bearing sports after a month.
Ankle replacement: office work can be resumed after 2 weeks, but if you do manual work you will need to wait until you have built up enough strength in your ankle after the cast, or external frame has been removed (4-5months). You should be able to drive once the cast has been removed (4 weeks) and start light sporting activity (swimming, cycling). High impact sports are not advisable due to the risk of injury and damage to the prosthesis.
Fusion: office workers can go back to work after 2 weeks, although manual workers will need to wait until they can walk properly which may be 3-4 months, depending on their recovery. You will be unable to drive until after the cast/external frame has been removed i.e. 8-12 weeks after the operation, when you can also resume non weight-bearing sports (cycling, swimming etc.). Due to the limited movement of your joint, it will not be possible to participate in other sports.